|
Diabetes doesn’t only prevent the patient from eating sweets and sugary foods but also destroys the core body part required for munching and chewing these foods-teeth! Diabetes rates have doubled or tripled in the last couple of decades everywhere around the world affecting not only the patient’s quality of life but also putting him/her at an elevated risk of multiple complications such as neuropathy, eye damage, skin disease, cardiovascular disease and periodontal disease. Periodontitis (a chronic inflammation disease of the mouth that involves the gingiva (gum tissues), teeth and supporting bone) has been identified as the sixth complication of diabetes and the sixth most common disease globally.
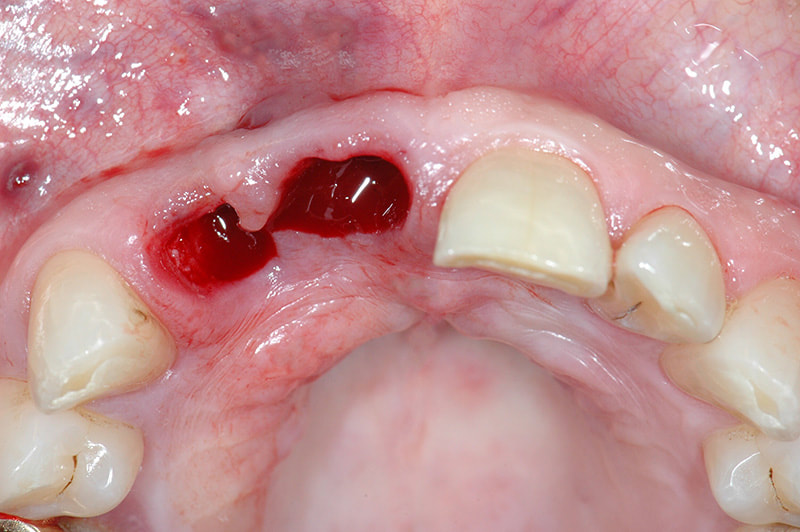
Periodontitis This is one of the most common diseases prevalent among humans. Though the progression of the disease is quite slow the tissue destruction that happens is largely irreversible. The disease is not painful during the initial stages which makes the person vulnerable to teeth damage and the patient recognizes the presence only after the condition had progressed enough to affect tooth mobility. In the early stages known as gingivitis the gums become swollen, red and might bleed whereas in the serious form called as periodontitis the gums might even pull out of the tooth, bone might be lost and the teeth might loosen and even fall away. While diabetes exists as a risk factor for periodontitis the presence of it increases the risk of stroke, myocardial infarction, atherosclerosis and hypertension. It can even cause delayed memory and calculation abilities in patients over the age of 60 and above. Those individuals with elevated blood glucose levels and diabetes mellitus display higher degrees of periodontal inflammation which often prove difficult to manage glucose levels due to persistent inflammation. It’s been proclaimed that diabetes exacerbates the onset, progression and severity of periodontitis. The intensity of the disease depends on how well the patient manages blood glucose levels. Diabetes patients have compromised immunity that puts them at a higher risk of infections, display decreased healing power and are at an increased risk of problems with the kidneys, eyes and heart-all these puts the person at a higher risk of periodontal disease. Such poor defence strategy can lead to higher risk of tooth loss in diabetes patients. Various studies help us understand the close-knit link between diabetes and periodontal disease in a better way. Retrospective Study The study below focused on 100 individuals (inclusion criteria included that the participants were above the age of 20 and suffered from diabetes) of which 50 of them suffered from diabetes and the rest were taken as the control group. India is one of the top countries with leading number of diabetes cases-while only 2.1% people suffered from diabetes mellitus in 1970s the rate has now risen to 12.1% which has a huge impact. The World Health Organization (WHO) has given a warning that India would become the ‘Diabetes Mellitus Capital of the World’ if we continue at this present rate. The present study shows that there is a significant difference in tooth loss among diabetics and non-diabetics. In another study done by Ogunbodede et al the female:male ratio was proved showing that females are the greater affected lot compared to males. Another study done by Chineye et al showed that male to female ratio in the diabetic subjects was 2:1. Some other studies showed male to female ratios as 1:1. A study done by Ochao et al at Columbia showed that there were 47.4% diabetic subjects who had a greater number of missing teeth and also suffered from gingival disease in the past. Periodontitis & Diabetes Can Affect Each Other Risk of periodontitis is almost 3-times greater in diabetics compared to others and the degree of the disease depends on the amount of blood sugar levels in the body. The US National Health & Nutrition Examination Survey (NHANES) III showed that adults with >9% Hb1A1C levels had higher prevalence of severe periodontitis compared to those without diabetes. There have been a number of case-controlled studies and all of them show that the risk of periodontitis is three-folds more in the Pima Indian population who suffered from diabetes mellitus compared to those who did not. Type 2 diabetes was considered to be the culprit for periodontitis but a couple of studies showed that type 1 diabetes also is an equal risk factor for the disease. One of the studies even proved that around 10% of kids (<18 years) with type 1 diabetes had profound bone and teeth loss compared to controls and another study on 350 diabetic kids aged 6-18 years and 350 non-diabetic kids showed that occurrence of periodontitis was greater in children with diabetes (20%) compared to controls (8%). Of late, we have emerging evidences that the link between diabetes and periodontitis is like a two-way channel-not only diabetes is a risk factor for periodontitis but also periodontal disease is a risk factor for diabetes. The Gila River Indian community was the first classic example to support the two-way theory. It showed that sever periodontitis was linked to a 9% increase in diabetes risk. The study also probed into the effect of periodontitis on overt nephropathy on 529 individuals aged ≥25 years who suffered from type 2 diabetes mellitus but no macroalbuminuria. It was seen that the incidence of macroalbuminuria was 2.0, 2.1 and 2.6 times higher compared to those with moderate or severe periodontitis. A 7-year prospective study on 5,848 diabetes-free individuals aged 30-59 years analysed the impact of periodontitis on diabetes incidence rates. Results showed that moderate-severe periodontitis increased the risk of diabetes incidence but the significance of it was lost after adjusting for sex, BMI, smoking, BMI, hypertension and HDL cholesterol. Another 5-year study looked into the effect of periodontitis on changes in HbA1C levels on 2,973 non-diabetic individuals. Results showed that participants with advanced periodontits at baseline showed 5-times greater increase in HbA1C levels over the 5 years compared to those with no periodontitis at baseline. This was the first study to show increase in HbA1C levels in those individuals who showed no signs of diabetes but only because they suffered from periodontitis. Such individuals who suffer from both diabetes and periodontitis are at a higher risk of cardiorenal mortality compared to those without severe periodontitis. A recent study looked at a 40-year trend of diabetes and periodontal disease collecting data from nine waves of National Health and Nutrition Examination Survey conducted from 1971 to 2012. 37,609 participants aged >25 years were involved and results showed that tooth loss was associated with diabetes. Both Diseases Have Inflammation as their Common Ground Periodontitis is a chronic inflammatory disease while both type 1 and type 2 diabetes increase systemic markers of inflammation. Elevated serum levels of IL-6 and TNF-α are seen in diabetes and the same is also seen in those affected by periodontitis. Such inflammation that’s linked with periodontal disease might also increase diabetes risk. Diabetes was consistently higher among Hispanic blacks and Mexican Americans than among non-Hispanic whites and the number of tooth lost after the age of 60 was higher among these three ethnic groups. The oral cavity has a diverse range of microbiota. Generally, the bacterial infection in periodontitis does not differ between nondiabetic and type 2 diabetes patients but there is a difference in the way the immune system responds. A study on 282 subjects (9% of them had type 2 diabetes) with similar severity of periodontitis showed that patients with type 2 diabetes might have fewer bacteria in periodontal pockets but with the same severity of the disease. The inflammatory response to infection in those suffering from type 2 diabetes is more compared to non-diabetic subjects. The accumulation of advanced glycation end-products (AGEs) in the periodontal tissues can also instigate periodontal inflammation in individuals with diabetes. AGE binds to its receptor (RAGE) producing inflammation mediators such as interleukin-6 and TNF- α. AGE increases oxidant stress, enhances respiratory burst in PMNs, has devastating effect on bone metabolism and alters lipid mechanism. Periodontal Treatment Improves Diabetes Levels There are various studies supporting the fact that periodontal intervention has positive effects on blood glucose levels. A combined report on 10 intervention studies on 456 patients showed a 0.66% decrease in HbA1C as a result of periodontal therapy. Another meta-analysis involving nine studies in 2008 showed 0.46% reduction in Hb1AC after treatment for periodontitis. A meta-analysis of 5 studies in 2010 involving 371 patients reported a reduction in Hb1AC of .40%. It was seen that in patients with A1C levels > 9.0% periodontal therapy reduced A1C by 0.6% in the absence of changes in medication and by 1.4% when diabetes medications are introduced. Though the logic behind reduction in glycemic levels post periodontal treatment is not clear researchers believe that it is due to reduced systemic inflammation. Reduction in Hb1AC levels greatly reduce the risk of diabetes complications-each 1% reduction in Hb1AC is associated with reduction in risk of 21% for any endpoint related to diabetes, 21% for deaths related to diabetes, 14% for myocardial infarction and 37% for microvascular complications. Diabetes is a significant risk factor for periodontitis and controlling diabetes controls the risk of periodontitis. The importance of oral health must be promoted in people with diabetes to avoid the consequences of tooth loss later. Many people remain unaware of the relationship between periodontitis and diabetes. Healthcare providers should check on a diabetes patient’s dental health and also suggest that the individual maintains oral hygiene to escape from the clutches of periodontitis and other dental health problems. References Prevalence of Periodontal Disease and Tooth Loss in Patients Suffering from Diabetes: http://www.medicalsciencejournal.com/archives/2019/vol5/issue1/5-1-94 Diabetes & Periodontal Disease: An Update for Healthcare Providers: https://spectrum.diabetesjournals.org/content/24/4/195 Periodontitis & Diabetes: A Two-way Relationship: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3228943/ Diabetes Linked to Increased Risk of Tooth Loss: http://www.diabetesincontrol.com/diabetes-linked-to-tooth-loss/ The Burden of Diabetes, its Oral Complications & Their Prevention & Management: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6108795/#ref81 Comments are closed.
|
AVOID FRAUD. EAT SMART+91 7846 800 800
|
- Home
- Written Testimonials
- Consult
- Clinics
- Blogs
-
Diet & Nutrition
- Diabetes Reversal
- IVF IUI not needed for PCOS PCOD Infertility
-
Medical Nutrition
>
-
Disease & Conditions
>
- Infertility | PCOS
- Diabetes Mellitus
- Cholesterol
- Hypothyroid
- Kidney Problems
- Hypertension
- Cardiovascular Diseases
- Liver Diseases
- Gastro intestinal disorder
- Cancer
- Metabolic Disorders
- Orthopedic Disorders
- Eating Disorders
- Dietary Recall
- Weight Record Filled By Clients
- Online Payment Transaction Details
- Online Clients Weight Check Form
- Our Program Package Service Charges
- Weight Record 2017 Clients
- Measurements sent by Clients
- Terms & Conditions Of Payment
- Thanks. Your Form is Submitted
- Video Testimonials
- Lifestyle & Wellness
- Lifestyle & Wellness Blog
- Allergy & Intolerance
- Weight Loss / Gain
- Weight Loss / Slimming Blog
-
Disease & Conditions
>
- Life Cycle Nutrition >
- Sports Nutrition >
- Integrity in Nutrition
- Knowledge Centre
© COPYRIGHT 2022. ALL RIGHTS RESERVED. FRST HEALTHCARE PVT LTD.
Dr. Nafeesa Imteyaz of First Eat Right clinic, is the Best Dietitian Nutritionist in Bangalore. Best Dietitian Nutritionist in Pune. Best Dietitian Nutritionist in Hyderabad. Best Dietitian Nutritionist in Chennai. Best Dietitian Nutritionist in Mumbai. Best Dietitian Nutritionist in Delhi. Best Dietitian Nutritionist in Kolkata.