|
Mankind is engulfed by stress existing as a result of our different actions, thoughts and deeds. Even kids and adolescents are swarmed by loads of homework or class projects that need their undivided attention most of the times; both the couples work equally hard to pull through the month which leaves the kids at the mercy of daycare and the unending rise in commodity prices has left us all agape with many families trying to end their lives unable to match their salary with the daily life requirements. Choices are many but so are the consequences of advancements. Stress at workplace is becoming even more troublesome than before and individuals sought for retirement as early as their early 50s unable to bear workplace stress. Such stress-related problems in workplace are present globally, costs every country’s economy millions of dollars annually and its effect is wide-spread at the occupational, personal and societal levels.
Occupational stress has the ability to affect our quality of life at every level-it prevents us from delivering excellent work or meet demands at workplace, increases the number of leaves taken, productivity is lost and the expenses incurred due to mental and physical health issues are costly. But when we analyze the underlying cause behind such occupational stress in the first place, it is primarily due to the inability of the individual to carry out the overwhelming demands of the workplace. When there is overpouring work, the individual loses his/her ability to deal with stress and this is further aggravated by poor diet routines that once again decrease our body’s ability to deal with stress. Food has always played an integral role in affecting the quality of life of individuals as it has the ability to improve cognitive skills and decrease negative moods such as depression, anxiety and stress. While different foods prove to be advantageous in different ways vitamins and minerals, especially B vitamins are great against diseases and disabilities. B vitamins play an essential role in various cortical processes involved in metabolism such as in the methylation of homocysteine to methionine that’s absolutely necessary for DNA synthesis, repair and other methylation reactions in the central nervous system. When this methylation process is disrupted it increases the likelihood of inflammation, oxidative stress and damage to mitochondria and DNA strands. Studies Related to Vitamin B Supplements Acting Against Stress The world now runs on medicines and supplements to pull us through everyday hurdles. Right from small kids to elderly people most of the individuals worldwide rely on supplements for strength and vitality as we all follow haphazard lifestyle practices and irregular eating patterns that’s hard on our body. Despite the widespread consumption of these vitamins and supplements we don’t have many clinical trials or research conducted analyzing the impact of these multivitamins on psychological strain. 2 studies observed reduction in stress levels after multivitamin supplements were given for 28 and 30 days. In one study, Schlebusch and colleagues used a well-designed protocol and screened for a highly stressed sample which after a duration of 30 days reduced stress and improved well-being. Another research team, Carroll and colleagues employed 80 male participants who were supplemented over 28 days and results showed that these participants witnessed reduction in stress levels compared to the placebo group. There are numerous advertisements shown for various supplements but their impact on human health is not proved without doubt. A research team analyzed whether a multivitamin supplement available in Australia that mainly consisted of B vitamins was helpful in improving work related stress after administering it for 90 days. 60 participants were recruited for the study and all of them completed a 3-month, double-blind, randomized, placebo-controlled trial in which each of the individual’s mood, anxiety, demands and strain were assessed. Results showed that the intervention group experienced significant reduction in personal strain from weeks 4 to 12 while the placebo group experienced an increase in strain from weeks 4 to 12. A double-blind, randomized, placebo-controlled Australian study tried to understand the relationship between B-vitamin supplementation, workplace stress and mood measures and also wanted to analyze whether dispensing vitamin B supplements for around 6 months had the ability to improve stress-related problems in healthy, working individuals. The study group’s secondary aim was to examine the mechanisms underpinning any mood or workplace stress enhancing actions of B vitamins by looking at the relationship between cognitive, biological and cardiovascular variables over these 6 months. The team chose 200 full-time participants who were aged between 30 and 65 years and reported feeling stressed in the workplace. The team excluded those individuals who suffered from psychiatric or neurological disorders, disorders affecting food metabolism, had diabetes, consumed alcohol regularly, suffered vision problems or suffered from chronic diseases. They also ruled out those participants who were pregnant, breastfeeding or planning to become pregnant, were taking anticoagulation meds or psychoactive meds that included antidepressants, antipsychotics, anxiolytics, illicit drugs or significant cognitive enhancing drugs. All the participants were asked to fill five online questionnaires and were screened over the telephone for their eligibility in participating in the study. Blood samples were collected and all of them were given a light breakfast before completing a cognitive test battery. All of them underwent two testing sessions at the end of which each of them were provided with supplements that could last for as much as 6 months. All the participants were asked to comment on their mood, stress levels and general health from the first to fifth month post randomization and during their second visit at the end of study period all of them were asked to return any unused supplements, if any. Primary outcomes measured include the effect of supplements on work-related stress while secondary outcomes include measuring cognitive stress, mood, health, personality, cardiovascular, biochemical, genetic and neuroimaging measures. Stress was assessed with the help of numerous self-reported questionnaires that will be used to assess stress, mood and general health. Stress symptoms were analyzed using a perceived stress scale (PSS), depression and anxiety was measured using the Beck Depressive Inventory II (BDI-II) and the Spielberger State-Trait Anxiety Inventory respectively. Dietary habits were inferred using a food frequency questionnaire. Results Separate mixed linear models were conducted to test the effects of treatment group (active vs. placebo) and time (baseline vs. 6 months) on blood plasma concentrations of homocysteine, vitamin B6, vitamin B12 and red blood cell folate. The treatment group had significant vitamin B6 and B12 concentrations indicating that the biomarker levels increased after treatment. There was a significant group by time interaction for plasma homocysteine concentration with the treatment group resulting in significantly reduced homocysteine but folate levels did not change as a result of treatment. The treatment also led to an increase in PCC (NAA, choline and creatine) concentrations. The study showed that 6 months intervention with B vitamin supplements increased plasma vitamin B6 and B12 levels and reduced blood plasma homocysteine levels. Vitamin B6 levels were associated with increased choline and creatine whereas increased B12 levels were linked to increased creatine concentrations. All these provide a green signal for the use of B vitamin supplements in reducing inflammation and oxidative stress and promoting neural metabolic processes. This is the first study to show the efficiency of high-dose B vitamin multivitamin supplementation in modulating the relationship between neural and blood biomarkers of oxidative stress. The supplementation helped in reducing the blood markers for oxidative stress and increasing the brain markers for oxidative metabolism and myelination. B vitamins definitely play an integral role in regulating brain health, keeping us from getting stressed and alleviating diseases and disability. A meta-analysis of eight studies that focused on the effect of multivitamins on mood and psychological state found that supplementing individuals with B vitamins reduced perceived stress, mild psychiatric symptoms and anxiety. References Reducing Occupational Stress with a B-vitamin Focused Intervention: A Randomized Clinical Trial: https://nutritionj.biomedcentral.com/articles/10.1186/1475-2891-13-122 The Effect of a High-Dose Vitamin B Supplement on the Relationship between Brain Metabolism & Blood Biomarkers of Oxidative Stress: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6316433/ B Vitamins & the Brain: Mechanisms, Dose & Efficacy: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4772032/ Diabetes doesn’t only prevent the patient from eating sweets and sugary foods but also destroys the core body part required for munching and chewing these foods-teeth! Diabetes rates have doubled or tripled in the last couple of decades everywhere around the world affecting not only the patient’s quality of life but also putting him/her at an elevated risk of multiple complications such as neuropathy, eye damage, skin disease, cardiovascular disease and periodontal disease. Periodontitis (a chronic inflammation disease of the mouth that involves the gingiva (gum tissues), teeth and supporting bone) has been identified as the sixth complication of diabetes and the sixth most common disease globally.
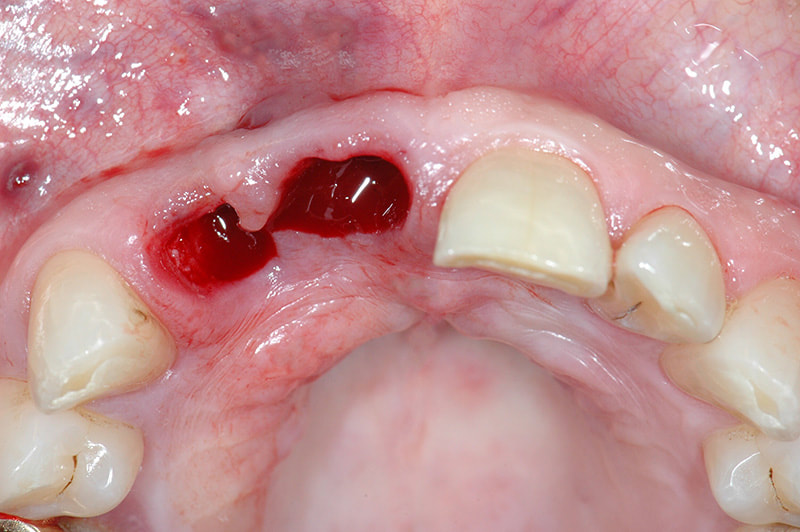
Periodontitis This is one of the most common diseases prevalent among humans. Though the progression of the disease is quite slow the tissue destruction that happens is largely irreversible. The disease is not painful during the initial stages which makes the person vulnerable to teeth damage and the patient recognizes the presence only after the condition had progressed enough to affect tooth mobility. In the early stages known as gingivitis the gums become swollen, red and might bleed whereas in the serious form called as periodontitis the gums might even pull out of the tooth, bone might be lost and the teeth might loosen and even fall away. While diabetes exists as a risk factor for periodontitis the presence of it increases the risk of stroke, myocardial infarction, atherosclerosis and hypertension. It can even cause delayed memory and calculation abilities in patients over the age of 60 and above. Those individuals with elevated blood glucose levels and diabetes mellitus display higher degrees of periodontal inflammation which often prove difficult to manage glucose levels due to persistent inflammation. It’s been proclaimed that diabetes exacerbates the onset, progression and severity of periodontitis. The intensity of the disease depends on how well the patient manages blood glucose levels. Diabetes patients have compromised immunity that puts them at a higher risk of infections, display decreased healing power and are at an increased risk of problems with the kidneys, eyes and heart-all these puts the person at a higher risk of periodontal disease. Such poor defence strategy can lead to higher risk of tooth loss in diabetes patients. Various studies help us understand the close-knit link between diabetes and periodontal disease in a better way. Retrospective Study The study below focused on 100 individuals (inclusion criteria included that the participants were above the age of 20 and suffered from diabetes) of which 50 of them suffered from diabetes and the rest were taken as the control group. India is one of the top countries with leading number of diabetes cases-while only 2.1% people suffered from diabetes mellitus in 1970s the rate has now risen to 12.1% which has a huge impact. The World Health Organization (WHO) has given a warning that India would become the ‘Diabetes Mellitus Capital of the World’ if we continue at this present rate. The present study shows that there is a significant difference in tooth loss among diabetics and non-diabetics. In another study done by Ogunbodede et al the female:male ratio was proved showing that females are the greater affected lot compared to males. Another study done by Chineye et al showed that male to female ratio in the diabetic subjects was 2:1. Some other studies showed male to female ratios as 1:1. A study done by Ochao et al at Columbia showed that there were 47.4% diabetic subjects who had a greater number of missing teeth and also suffered from gingival disease in the past. Periodontitis & Diabetes Can Affect Each Other Risk of periodontitis is almost 3-times greater in diabetics compared to others and the degree of the disease depends on the amount of blood sugar levels in the body. The US National Health & Nutrition Examination Survey (NHANES) III showed that adults with >9% Hb1A1C levels had higher prevalence of severe periodontitis compared to those without diabetes. There have been a number of case-controlled studies and all of them show that the risk of periodontitis is three-folds more in the Pima Indian population who suffered from diabetes mellitus compared to those who did not. Type 2 diabetes was considered to be the culprit for periodontitis but a couple of studies showed that type 1 diabetes also is an equal risk factor for the disease. One of the studies even proved that around 10% of kids (<18 years) with type 1 diabetes had profound bone and teeth loss compared to controls and another study on 350 diabetic kids aged 6-18 years and 350 non-diabetic kids showed that occurrence of periodontitis was greater in children with diabetes (20%) compared to controls (8%). Of late, we have emerging evidences that the link between diabetes and periodontitis is like a two-way channel-not only diabetes is a risk factor for periodontitis but also periodontal disease is a risk factor for diabetes. The Gila River Indian community was the first classic example to support the two-way theory. It showed that sever periodontitis was linked to a 9% increase in diabetes risk. The study also probed into the effect of periodontitis on overt nephropathy on 529 individuals aged ≥25 years who suffered from type 2 diabetes mellitus but no macroalbuminuria. It was seen that the incidence of macroalbuminuria was 2.0, 2.1 and 2.6 times higher compared to those with moderate or severe periodontitis. A 7-year prospective study on 5,848 diabetes-free individuals aged 30-59 years analysed the impact of periodontitis on diabetes incidence rates. Results showed that moderate-severe periodontitis increased the risk of diabetes incidence but the significance of it was lost after adjusting for sex, BMI, smoking, BMI, hypertension and HDL cholesterol. Another 5-year study looked into the effect of periodontitis on changes in HbA1C levels on 2,973 non-diabetic individuals. Results showed that participants with advanced periodontits at baseline showed 5-times greater increase in HbA1C levels over the 5 years compared to those with no periodontitis at baseline. This was the first study to show increase in HbA1C levels in those individuals who showed no signs of diabetes but only because they suffered from periodontitis. Such individuals who suffer from both diabetes and periodontitis are at a higher risk of cardiorenal mortality compared to those without severe periodontitis. A recent study looked at a 40-year trend of diabetes and periodontal disease collecting data from nine waves of National Health and Nutrition Examination Survey conducted from 1971 to 2012. 37,609 participants aged >25 years were involved and results showed that tooth loss was associated with diabetes. Both Diseases Have Inflammation as their Common Ground Periodontitis is a chronic inflammatory disease while both type 1 and type 2 diabetes increase systemic markers of inflammation. Elevated serum levels of IL-6 and TNF-α are seen in diabetes and the same is also seen in those affected by periodontitis. Such inflammation that’s linked with periodontal disease might also increase diabetes risk. Diabetes was consistently higher among Hispanic blacks and Mexican Americans than among non-Hispanic whites and the number of tooth lost after the age of 60 was higher among these three ethnic groups. The oral cavity has a diverse range of microbiota. Generally, the bacterial infection in periodontitis does not differ between nondiabetic and type 2 diabetes patients but there is a difference in the way the immune system responds. A study on 282 subjects (9% of them had type 2 diabetes) with similar severity of periodontitis showed that patients with type 2 diabetes might have fewer bacteria in periodontal pockets but with the same severity of the disease. The inflammatory response to infection in those suffering from type 2 diabetes is more compared to non-diabetic subjects. The accumulation of advanced glycation end-products (AGEs) in the periodontal tissues can also instigate periodontal inflammation in individuals with diabetes. AGE binds to its receptor (RAGE) producing inflammation mediators such as interleukin-6 and TNF- α. AGE increases oxidant stress, enhances respiratory burst in PMNs, has devastating effect on bone metabolism and alters lipid mechanism. Periodontal Treatment Improves Diabetes Levels There are various studies supporting the fact that periodontal intervention has positive effects on blood glucose levels. A combined report on 10 intervention studies on 456 patients showed a 0.66% decrease in HbA1C as a result of periodontal therapy. Another meta-analysis involving nine studies in 2008 showed 0.46% reduction in Hb1AC after treatment for periodontitis. A meta-analysis of 5 studies in 2010 involving 371 patients reported a reduction in Hb1AC of .40%. It was seen that in patients with A1C levels > 9.0% periodontal therapy reduced A1C by 0.6% in the absence of changes in medication and by 1.4% when diabetes medications are introduced. Though the logic behind reduction in glycemic levels post periodontal treatment is not clear researchers believe that it is due to reduced systemic inflammation. Reduction in Hb1AC levels greatly reduce the risk of diabetes complications-each 1% reduction in Hb1AC is associated with reduction in risk of 21% for any endpoint related to diabetes, 21% for deaths related to diabetes, 14% for myocardial infarction and 37% for microvascular complications. Diabetes is a significant risk factor for periodontitis and controlling diabetes controls the risk of periodontitis. The importance of oral health must be promoted in people with diabetes to avoid the consequences of tooth loss later. Many people remain unaware of the relationship between periodontitis and diabetes. Healthcare providers should check on a diabetes patient’s dental health and also suggest that the individual maintains oral hygiene to escape from the clutches of periodontitis and other dental health problems. References Prevalence of Periodontal Disease and Tooth Loss in Patients Suffering from Diabetes: http://www.medicalsciencejournal.com/archives/2019/vol5/issue1/5-1-94 Diabetes & Periodontal Disease: An Update for Healthcare Providers: https://spectrum.diabetesjournals.org/content/24/4/195 Periodontitis & Diabetes: A Two-way Relationship: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3228943/ Diabetes Linked to Increased Risk of Tooth Loss: http://www.diabetesincontrol.com/diabetes-linked-to-tooth-loss/ The Burden of Diabetes, its Oral Complications & Their Prevention & Management: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6108795/#ref81 Man is addicted to habits and a slight change in his/her daily routine frustrates and puts him/her at unease. Think about a baby who lives inside his/her mother’s womb for nine whole months and comes unto this world full of hopes and surprises! There would be a change in temperature, environment and what not-being brought into this world, the newborn is now faced with the challenges of accommodating from intra-uterine to extra-uterine. According to the World Health Organization (WHO) the early newborn period is most critical for survival of a neonate (the period right from birth up to 28 days of age) and the child is probably at the highest risk of death during this period in a world where close to 10 million deaths occur every year in kids younger than 5 years old. Almost two-thirds of such deaths happen in the neonatal period where one-third of them happen during the first day of life of the neonate, almost half within 3 days and nearly three-quarters within first week of life. Developing countries contribute to a majority of such deaths with almost 34 of every 1000 live births leading to death and our country has seen a steady decline in the number of neonatal deaths from around 53 to only 22-28 per 1000 live births. Sub-Saharan Africa ranks highest in such deaths where the child’s day of birth is also its day of death unfortunately.
Death doesn’t occur all of a sudden mostly and there are multiple clinical signs that lead to the fatality. Fever is a common manifestation of diseases and requires immediate medical attention. Other signs include lethargy, poor sucking, increased respiratory rate (more than 60 beats per min), chest retractions and convulsions (sudden, abnormal electrical activity in the brain). Hence, the first 28 days are like a test to the child’s survival-it is of utmost importance to provide the best of feeding and care to maximize the neonate’s chances of survival and a healthy existence in this world. Developed by UNICEF and WHO the Integrated Management of Childhood Illness (IMCI) approach is understanding the various underlying causes of illness. This recognition of danger signs by the parent or any other caretaker helps in getting medical attention as early as possible. The reason why there is so much insistence is because a majority of neonatal deaths occur at home in which almost 75% can be prevented if there was timely action taken, the signs of an illness recognized by the parent/caretaker and there was no delay in the choice to go for medical action. Here, in this article we would be looking at the parent’s knowledge about the kid’s health, changes in health and the capacity to seek medical help in countries around the world. Knowledge of Mothers Regarding their Neonate’s Health Status in Ethiopia As per 2016 records, under-5 mortality rates were 67 deaths per 1,000 live births and most neonatal deaths occur at home showing that still most are unable to recognize and give treatment at the right time. Most children die due to lack of knowledge of the parent and the research here assesses the mother’s knowledge on neonatal danger signs and the reasons behind such poor knowledge for being unable to save her dying neonate! 368 mothers were selected to participate in the study of which 355 of them completed the interview. Mean age of the participants was 27.7, almost 60% of them were housewives and 234 (65.9%) of them gave birth at health institutions. It was reported that of the 355 participants, 281 (79.2%) of them had information about neonatal danger sign of which diarrhea (160 were aware), fever (136) and persistent vomiting (127) were more familiar with the participants. It was seen that 68.68% moms had good knowledge about neonatal danger signs-they were familiar with three or more signs of danger. When asked about the place of care 78 mothers (33.8%) opted for home care of their sick neonate, 82 (32%) wanted to take them to health institutions, 56 (24.2%) wanted to take them to traditional healers and 15 (6.5%) did nothing. Home care was basically garlic, tenadam, a mix of lemon and ash applied on the neonate’s head for tonsils, matchstick for convulsion, tepid sponging for fever, sunlight exposure for jaundice and using coconut oil to rub all over the body for cold body. 118 mothers continued to breastfeed despite the presence of disease but 113 of them did not. The factors associated with the mom’s knowledge include the mom’s educational status, income, place of birth and source of information. Moms who gave birth in a health institution were 6.45 times likelier to take their neonates back to the institution and those who received a post-natal care (PNC) follow were 6.19 times likelier to go back to the hospital for a follow up. It was also seen that husband’s education status, husband occupation status, place of birth and PNC had a significant effect on the maternal practice for neonatal danger signs. The study clearly showed that educational qualification and work status clearly dominated the list of attributes that motivated women to seek the help of a health institution. Another study in Ethiopia on 400 mothers/caregivers had a response rate of 94.7% and the participants’ mean age was between 25 and 34 years. Almost 64% were illiterate mothers with only 7.5% completing secondary education. Almost 40% infants were between 9 and 24 weeks of age, 32% were between 8 and 16 weeks of age and only 5.5% were aged less than one week during the study period. 67.5% infants were delivered at the hospital and only 6.6% of them were delivered at home. Of the study group almost 92.8% of them reported that they take their children to the health care center and among the rest who don’t almost 34% reported high treatment cost followed by lack of money (30%) as the reason behind it. When the study group tried to categorize the mother’s knowledge about their neonate’s risk as adequate and inadequate it was observed that almost two-thirds (65.3%) of them had inadequate knowledge as they were not even able to identify more than three symptoms among the 13 symptoms of illness of newborns and young infants. Knowledge of Mothers Regarding their Neonate’s Health in India Neonatal mortality rates (NMR) have dropped significantly in our country with Uttarakhand having a minimum of 11 and Haridwar having maximum NMR of 50. In Dehradun, neonatal mortality rate is 32 per 1000 live births. The survival of the child depends on the mother’s health alongside her knowledge and skills as a mom is the ‘one’ person who has constant contact with the child monitoring his/her actions and health. The baby is said to be in danger when any of the following signs are experienced: movement only when stimulated, temperature below 35.5 °C and above 37.5 °C, respiratory rate over 60 breaths per minute, history of convulsions and history of feeding difficulty. The study conducted in Dehradun included 100 mothers for sampling but only 53 of them reported neonatal danger signs and were monitored for their observation and handling practices. Results showed that:
Knowledge of Mothers Regarding their Neonate’s Health in Saudi Arabia Infant mortality rate in Saudi Arabia is pretty low-11 deaths per 1000 live births as per 2015 results. Under-five mortality rates in this country has reached Millennium Development Goal-4 target still infant mortality rates remains higher compared to many other countries. A community-based study was conducted in Riyadh city of this country regarding a mother’s knowledge about WHO guidelines on neonate danger signs. Primary health care centers (PHCC) are located all over the city and they provide free care to most of the residents there. Sample data of all the mothers who delivered a baby or nursed a baby (as in the case of caregivers such as grandmothers, grandfathers, fathers or nannies) in the past two years were taken from these health care centers. Face to face interviews were conducted with the mothers-the mother’s knowledge and her response on the neonate’s danger signs was collected, all the participants were asked to list the signs that they found threatening to the neonate’s life, recall any signs of danger that they personally experienced with the neonate, the time from noticing any danger to presenting it at the health facility, care received at the society and outcome of the neonate’s illness. A total of 1428 women who were in the age group of 20-60 years were included in the study. 98% neonates were cared by their mothers, 33% had education up to degree level and 37% had secondary education. 87% women had attended antenatal care and 45% had 4 or more children. Results showed that:
Research Mother’s Knowledge & Practice about Neonatal Danger Signs & Associated Factors: http://www.jbiomeds.com/biomedical-sciences/mothers-knowledge-and-practice-about-neonatal-danger-signs-and-associatedfactors-in-wolkite-town-gurage-zone-snnpr-ethiopia-2017.php?aid=21314 Neonatal Danger Signs: Attitude & Practice of Post-natal Mothers: https://www.omicsonline.org/open-access/neonatal-danger-signs-attitude-and-practice-of-postnatal-mothers-2167-1168-1000401.php?aid=89908 Mother’s & Caregiver’s Knowledge on Neonate’s Danger Signs: https://www.hindawi.com/journals/bmri/2019/1750240/ Parents’ Knowledge of Danger Signs & Health Seeking Behavior in Newborn & Young Infant Illness in Southwest Ethiopia: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6308740/ Metabolic syndrome (MetS) is a cluster of metabolic disorders that increase the risk of cardiovascular disease when present in combination with each other. The disorders that elevate the risk include hypertension, central obesity, glucose intolerance and serum lipid disorders. While these conditions are good enough to put the individual in a high-risk category for heart problems there is a greater chance that the individual could suffer from cardiovascular issues when they occur in together. There has been an increasing concern regarding MetS as more than 23% of the adult population seems to be affected making them susceptible to diabetes, cardiovascular disease, stroke and diseases related to fatty build-up in artery walls. So, when we look at the risk factors behind this disease its none other than obesity, overweight, physical inactivity, genetic factors and ageing.
Its been found that certain MetS features such as excessive adiposity, dyslipidaemia and glucose intolerance are strongly associated with depression-a health condition that now exists as the fourth biggest cause of disease burden in the world. Women are the primary victims of this condition though these days increasing number of men silently suffer from its effects. Depression involves change in mood and cognitive function besides being linked to a proinflammatory process that increases the risk of being affected by cardiovascular disease. There is a widespread prevalence of an activated peripheral immune system in these adults with overproduction of proinflammatory cytokine that has the potential to increase the risk of depressive symptoms. As it is now evident that both MetS and depression are commonly present bearing increased public health implications there has been interests shown in finding out an association between them. Depression involves dysregulation of the adrenocortical and autonomic nervous systems both of which increase the risk of MetS by supporting abdominal fat accumulation and insulin resistance. MetS is generally linked to increased levels of inflammatory cytokines and leptin resistance and c-reactive protein (CRP) is one of the commonly present inflammatory markers in subjects with MetS. Health experts have come up with various proposals for controlling MetS occurrence the most common of which includes lifestyle changes (that includes diet modifications and exercises) and drug therapy. The Mediterranean diet has been generally prescribed as the best weight loss approach that’s beneficial for both MetS and depression. But we do have questions arising on how weight loss can have a positive effect on the mind in terms of reducing symptoms of depression. The study below exactly deals with this concern-it uses a subsample of the RESMENA-S study that tries to reduce MetS using a hypocaloric diet for a period of six months. It was generally assumed that the this diet does have a positive effect on depressive symptoms as well and the research team tried to understand the process through which it happens. RESMENA-S Study The study included 93 subjects (52 men and 41 women) aged around 50 years with a BMI around 36 kg/m2 diagnosed with MetS. Six months after following the hypocaloric diet 26 participants were eliminated due to different reasons and 7 of the 67 participants who did complete the study did not finish the Beck Depression Inventories (BDI) and hence, the study was left with not more than 60 participants who were able to complete the BDI in three visits (at baseline, after two months and end of six months). All the participants were put into either of the two groups randomly-control group or the RESMENA diet. All the participants were requested to carry on with their regular physical activity schedules and their performance was measured using a 24-hour physical activity questionnaire at the beginning and end of study. The research team measured serum glucose, total cholesterol, HDL-cholesterol, triglycerides and free fatty acids serum concentration. Depression symptoms were analysed thrice over the course of the study (at baseline, after two months and at the end of the study) using a Spanish version of the BDI. A score of ≥10 reflects moderate depressive symptoms. Results Results showed that:
References A Decline in Inflammation is Associated with Less Depressive Symptoms after a Dietary Intervention in Metabolic Syndrome Patients: https://nutritionj.biomedcentral.com/articles/10.1186/1475-2891-13-36 Systematic Inflammation is Associated with Depressive Symptoms Differentially by Sex and Race: A Longitudinal Study of Urban Adults: https://www.nature.com/articles/s41380-019-0408-2 Postnatal depression was the only type of depression known to the world two decades back and those women suffering from antenatal depression were simply told that it’s just their hormone calling for attention. It’s been observed that 1 in every 10 women will be depressed at any point of time during pregnancy while 1 of every 30 women will be depressed during pregnancy and after delivery. Pregnancy, as we all know, is the most joyous period in a woman’s life as the pregnant woman experiences the peak of womanhood looking forward to the birth of her loving child. But according to some pregnant women who experience prenatal depression, the same pregnancy term instead of being filled with happiness and excitement turns out into a period of despair and gloom. There are various causes including physical, emotional and hormonal effects that can raises the risk of prenatal depression but this has dangerous consequences on the newborn, child and adult health outcomes putting the individual at a higher risk of common disorders.
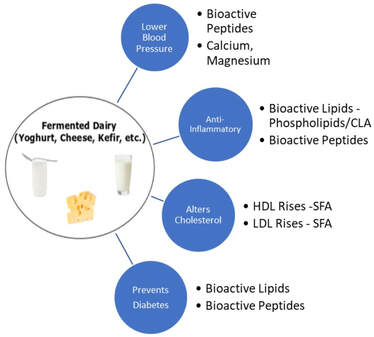
Disasters of Depression in Pregnant Women Depression as such is one of the highly common mental disorders that’s 50% more common in women than men. Almost 10-15% of women in developed countries and 20-40% of women in developing countries experience depression during pregnancy or after childbirth. Such depressions in pregnant women could have debilitating health outcomes when it is not stopped at the right time. Beyond affecting the immediate family, it also affects the society. Pregnancy is the period during which the woman undergoes numerous hormonal changes, her nutrient requirements vary and the mind goes through a sea of conflicting emotions simultaneously. We often hear elderly people advice the pregnant lady to eat for two as she is carrying another human inside but dietary guidelines don’t support this. Still, nutrient requirements increase to meet the needs of the developing fetus and the mother as well and fulfilling these requirements prepares the woman for a healthy delivery and a healthy baby thereafter. But depression brings about changes in her nutrient intakes which finally affects the health of the baby and the mother. Generally, these women eat fewer macronutrients (with the exception of fats), their nutrient levels are lower (with the exception of phosphorus) than recommendations and there are also theories that while these women have sufficient intake of macronutrients they witness a decrease in micronutrient intake. Often we see people eating according to their mood. We indulge in sweets when we are happy or even refrain from eating when we are sad. Some people cope up with sorrows in life by eating tubs of cheesy fries and it has been shown that mental health of women affects their nutritional intake and also impacts the fetus. Depressed women are at an increased risk of giving birth to neonates with low birth weight (LBW) (this is a leading cause of neonate mortality and morbidity), preterm birth or with an Apgar score of 1-5 some five minutes after birth. Women around the world suffer from antenatal depression with each of them experiencing different outcomes. A Study on Antenatal Depression in Pakistani Pregnant Women Pakistan has a maternal mortality rate of 260 for every 1,00,000 live births with almost 18-80% pregnant women suffering from antenatal depression. The study aimed at measuring association of depression with maternal dietary intake and neonate outcomes. Participants were pregnant women aged between 18 and 49 years at the start of their second trimester and having normal nutrient intakes. The study group ensured that those with depression, chronic diseases such as diabetes, anemia, BP and CHD or belonging to the high-risk pregnancy category were excluded from the study. Information about the participants such as demography, husband’s employment, gestational age and expected delivery date was collected using questionnaires. The Edinburgh Postnatal Depression Scale (EPDS) was used to measure the participant’s state of mind. Of the 94 participants who were cleared for the study 12 of them were excluded following no-show during follow up and finally the study was carried out with a sample size of 82. An EPDS score of 9 indicated absence of depression, a score of 9-12 indicated moderate depression and a score of more than 13 indicated severe depression. Maternal intake was noted using a 24-hour dietary recall and a Food Frequency checklist at the start of the study and the same was repeated at the 36th week of gestation to analyze poor maternal nutrient intake. Food items were classified and their frequency of consumption (between never and 6+ times in a week) was noted. Each of the participants were questioned on their methods of preparation, portion sizes consumed and the types of snacks eaten. The 24-hour dietary recall was used to calculate macronutrient intake. The Healthy Eating Index (HEI) was used to score the 24 h recall with the overall score being reduced to 50 with the score split based on the type of food consumed-total fruit (5 score), whole fruit (5 score), total vegetables (5 score), greens and beans (5 score), whole grain (10 score), dairy (10 score), total protein foods (5 score) and seafood and plant proteins (5 score). Following dietary guidelines protocol to the dot yielded full score, a score ≥40 indicated good diet, a score between 25 and 40 was rated as moderate and a score below 25 was considered poor diet. Cut off points for carbohydrate and protein intake were ≥175 g and ≥71 g while it was ≥55 g for fats. Height, weight and BMI measurements of all the participants were taken and each of them was classified as underweight, normal weight, overweight or obese based on WHO guidelines. Information on the newborn was acquired in the form of fetal growth retardation (FGR), low (score of 6 or less) Apgar score and low birth weight (LBW) scores (<2500 g). Result While mean age of the participants was 29 years almost 51% of them were between 24-29 years and 66% of them were between 151 and 160 cm. Mean weight of moms was 70 kg and BMI was 26.6. Results showed that there was a mean difference of only one HEI between depressed and non-depressed women as depressed antenatal women were consuming 151 kcal lesser than non-depressed women at the start. But at the end of the study, there was a difference of 5 HEI between depressed and non-depressed antenatal women. Depressed women ate almost 321 kcal lesser than non-depressed women by the end of cohort. At baseline, the type and quantity of foods consumed by both categories (depressed and non-depressed) of women were almost similar. While consumption of cereal, beans and lentils remained almost constant even after succumbing to antenatal depression usage of eggs decreased drastically (by almost 43% initially up to 75% later). Though 85% women were drinking milk at the start of the study it dropped to 65% later. Similar changes were seen in fruits and vegetables intake too. 60% of depressed antenatal women consumed one serving of fruit at baseline but the figures decreased to 37% by the end of cohort. Sadly, none of them were having green leafy vegetables even once a week. It was seen that almost 62% of poor dietary intake was due to antenatal depression. Protein and fat intake in antenatal depressed women decreased to less than 71g and 55g at the end of cohort. Mean gestational age (born 2 days earlier), weight (200 g less) and low (0.5lower) Apgar score were low among neonates of depressed antenatal women compared to non-depressed women. FGR, preterm birth and poor Apgar score was predominantly seen among neonates of depressed antenatal women but not LBW and in this, 60% of FGR and poor Apgar score and 54% of preterm births could be attributed to antenatal depression. The study clearly reveals the impact of depression on the nutrient intake of pregnant women and dietary intake must be an important topic of discussion during nutrition counseling in the absence of which birth of a healthy baby and survival of a healthy mother both remain questionable. References Effect of Antenatal Depression on Maternal Dietary Intake & Neonatal Outcome: https://nutritionj.biomedcentral.com/articles/10.1186/s12937-016-0184-7 The Interplay between Maternal Nutrition and Stress during Pregnancy: https://www.karger.com/Article/PDF/457136  Choose your Favourite Fermented Dairy Food to Protect Your Body against CVD Risk Choose your Favourite Fermented Dairy Food to Protect Your Body against CVD Risk Do you remember the boy in the ad with a milk moustache? Then you are probably an 80s or 90s kid who has grown up seeing and hearing about the goodness of consuming dairy and its benefits on bone health-in those days dairy products were the magicians who could provide individuals with stronger bones and muscles. But today, the effects of dairy have been made dark and twisted with the food group being beneficial or harmful depending on the people’s intake and needs. While it might not be the best way to a healthy body dairy indeed is the simplest way to equip yourself with calcium, vitamin D and proteins to enable optimal functioning of the heart, muscles, bones and overall body. Kids are constantly forced to drink between 2 and 3 glasses of milk for sufficient calcium levels and one should also not forget the fact that bones become stronger only up to the age of 3 after which bone mass starts deteriorating. Hence, parents insist that their children consume dairy products like milk, cheese, yoghurt and cottage cheese for maintaining bone density and reducing risk of fracture. Fermented foods are the recent health craze and fermented dairy foods are no exception. Cheese and yoghurt are fermented foods that are a part of the Mediterranean diet, a diet that’s acclaimed for its protective nature against cardiovascular diseases (CVD). Dairy products have the capability to provide up to 60% of the recommended daily allowance (RDA) of calcium and fermented dairy products are an excellent source of vitamin K. We have studies showing that fermented dairy products show beneficial effects on blood lipid profiles and the risk of heart disease compared to regular dairy products as they deliver probiotics that benefit the gut microbiota. The human gut has been the centre of attraction these days as they seem to regulate whole body health. Still, there are not many research studies providing insightful data on the benefits of fermented dairy foods. Cardiovascular Benefits of Fermented Dairy Products on Australian Population Type 2 diabetes mellitus (T2DM) and CVD are spreading like forest fire worldwide and researchers are trying various means to curb their rise. Of late, there has been an increasing interest in the relationship between dairy consumption, specifically fermented dairy foods, and its effect on T2DM and CVD risk. We have meta-analysis from cohort studies showing that yogurt consumption has a positive effect on T2DM. Yet another meta-analysis of 29 cohort studies showed that consumption of fermented dairy products (such as milk products, cheese and yogurt) was inversely associated with CVD risk. There are not many studies that focus on middle-aged people as study participants and the Australian study discussed below examines the association between fermented dairy products and T2DM and CVD risk in Australian women. The Australian Longitudinal Study on Women’s Health (ALSWH) is a population-based cohort study examining the health and well-being of >58,000 Australian women. The current study included data from 1946-1951 age cohort and these women were surveyed every 2-3 years since the start of ALSWH in 1996. Information on dietary intake was first collected in survey 3 in 1991 and this was used as a baseline for the present study. Surveys 5-7 once again included dietary intake. After implementing various exclusion criteria, the study was left with 7633 participants in the T2DM subcohort and 7679 participants in the CVD subcohort. T2DM and CVD was self-reported and during every survey, women were asked whether they were diagnosed or treated for diabetes and coronary heart disease (CHD) in the past 3 years. In the present study, CVD was defined as the sum of CHD and stroke and incidence was defined as the onset of T2DM and CVD at surveys 4-8. Dietary intake was noted down with the help of a food frequency questionnaire (FFQ) that collected information on dairy consumption that included yogurt, cheese (different types of cheese such as hard cheese, soft cheese, firm cheese, ricotta or cottage cheese and low-fat cheese) and milk (including reduced-fat milk, skim milk, soya milk and flavoured milk). All the participants were asked to mark down their frequency of intake of dairy products over the last 12 months through the use of a 10-point scale (which has measurements from never to ≥3 times/d with the intake converted to grams per day) with milk being the only exception here whose intake quantity was reported between none and ≥750 ml/d. All the dairy products were classified as yogurt, total cheese (all types of cheese), total fermented dairy (sum of yogurt and total cheese), total nonfermented dairy (all types of milk) and total dairy (sum of total fermented dairy and nonfermented dairy). Women self-reported on height, weight and other body measurements; physical activity was calculated according to total metabolic equivalent (MET in min/wk) into ‘sedentary or low physical activity level’ (<600 MET min/wk), ‘moderate physical activity level’ (from 600 to <1200 min/wk) or ‘high physical activity level’ (≥1200 min/wk). BMI measurements were calculated and categorized as underweight (BMI <18.5), healthy weight (BMI from 18.5<25), overweight (BMI from 25-30) and obese (BMI ≥30). Results The mean age of 8748 women enrolled in the study was 52.5 years and mean BMI was 26.8. Women belonging to the highest tertile of energy-adjusted total dairy intake were likelier to have a lower BMI, were higher educated, never smoked, rarely drank and were physically active. Above all, they had a lower intake of total energy with median intakes corresponding to 20 g/d for yogurt, 14 g/d for total cheese, 35 g/d for total fermented dairy, 202 g/d for nonfermented dairy and 369 g/d for total dairy. 7633 were diabetes-free at baseline and were followed-up for ≤15 years. During follow-up 701 (9.2%) T2DM cases were reported. Results showed that:
Fermented Dairy Intake & CVD Disease Risk in Men Researchers at the University of Eastern Finland studied 2,000 men for their risk of CVD on consumption of fermented dairy products. All the participants’ dietary habits were assessed at the start of the study (1984-89) and followed up for around 20 years during which 472 of them experienced coronary heart disease event. All the participants were split into four groups depending on how much dairy (that is, fermented dairy products with less than 3.5% fat) they consumed and the researchers compared the groups with the highest and lowest consumption. Results showed that the incidence of coronary heart disease was 26% lower in the highest consumption group compared to the lowest consumption group, sour milk was the commonly used low-fat fermented dairy product and consumption of high-fat fermented dairy products such as cheese was not associated with coronary heart disease risk. On the other hand, increased consumption of non-fermented dairy products (such as milk whose intake was as high as 0.9 litre/day in some individuals) was associated with an increased risk of coronary heart disease. The practise of dairy consumption is changing all over the globe and in Finland (where this study happened) too people are moving away from the consumption of dairy products such as milk and sour milk to those fermented dairy products such as cheese, yogurt and others. Hence, men who eat plenty of fermented dairy products are at a reduced risk of CHD than men who eat less of these products. A study comparing fermented and non-fermented dairy products in a Swedish cohort found that there was a 32% increased hazard in consuming non-fermented milk compared to fermented milk. In another crossover-controlled study yoghurt consumption increased HDL levels in 29 hypocholesterolaemic women and we have other studies showing that fermented dairy intake has positive or neutral effects on fasting plasma glucose levels. Many studies revolve around the hypothesis that fermented dairy products induce cardioprotective effects due to the intake of bacterial metabolites and probiotics. Fermented dairy seems to be way better in every way compared to non-fermented dairy and individuals should take greater care to consume such products. References Total Fermented Dairy Food Intake is Inversely Associated with Cardiovascular Disease Risk in Women: https://academic.oup.com/jn/article/149/10/1797/5514556 Fermented Dairy Products May protect Against Heart Attack, Study Suggests: https://www.sciencedaily.com/releases/2018/10/181030102828.htm Dairy Fats and Cardiovascular Disease: Do We Really Need to be Concerned? https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5867544/ Fermented Dairy Food & CVD Risk: https://pdfs.semanticscholar.org/336d/1c0782de6bcf3ee2056c0481119e088380a2.pdf A Low-fat Diet During Menopause Causes Loss of Hope for Diabetes & Heart Disease to Take Over11/7/2019
Puberty and menopause bring in immense changes in a woman’s life which includes both physical and psychological. Her body undergoes staggering hormonal changes which in turn affect her body weight and food intake patterns too. Every girl needs immense care and comfort during her puberty years and every woman needs support and understanding nearing menopause. Ageing can increase body weight despite the individual eating the same number of calories as before. When menopause affects woman alongside ageing it causes double trouble-there are more chances of weight gain around the abdomen especially which pave way for an increased risk of diseases and health problems. Menopause is an indication that the ovaries make very little estrogen and such reduced estrogen levels increase the risk problems such as heart disease, stroke, osteoporosis and urinary incontinence in the years following menopause. Stringent dietary modifications and regular physical activity is recommended to avoid unnecessary weight gain changes in the absence of which overweight/obesity might be a common occurrence.
Diets low in saturated fats and cholesterol are associated with lower CVD rates and studies show that a Mediterranean-type dietary pattern (low-fat dietary pattern) prevented the occurrence of cardiovascular events. Women’s Health Initiative Dietary Modification Trial The main aim of the Women’s Health Initiative (WHI) Dietary Modification Trial was to understand whether a dietary pattern low in total fat alongside increase in the intake of vegetables, fruits and grains would decrease the risk of breast and colorectal cancer in postmenopausal women. The secondary aim was to note any link between such dietary intake and reduced risk of CVD. A total of 48,835 women aged between 50 and 79 years were enrolled between 1993 and 1998 in 40 US clinical centres and assigned to either the intervention group (40%) consisting of 19541 participants or the usual-diet comparison group (29,294 participants). While inclusion criteria stated being postmenopausal and consuming fat intake of 32% of total calories exclusion for WHI included prior occurrence of breast or colorectal cancer, medical conditions with survival rate less than 3 years and habits such as alcoholism. People with type 1 diabetes and those eating meals frequently away from home were also included in the exclusion list. All the participants were monitored for their total fat, vegetable, fruit and whole grain intake, they were supplemented with group activities and were also invited to participate in any one of the WHI controlled trials of hormone therapy (HT). Participation in a trial of calcium and vitamin D supplementation (CaD) was offered after one year. In total, 20,592 (42.2%) participated in the Dietary Modification Trial, 8050 (16.5%) in the Dietary Modification plus HT Trial, 25,210 (51.6%) in the Dietary Modification plus CaD Trial and 5017 (10.3%) in all 3 trials. All the participants were contacted bi-annually for changes in health outcomes while height, weight and BMI measurements were taken annually. Electrocardiograms (ECGs) were taken every 3 years, a medical update questionnaire was given every 6 months to fill and CHD, the outcome variable involved in the study was defined as acute myocardial infarction (MI) that required hospitalization. Adherence assumption included 13% lower consumption of fats in the intervention group compared to the control group one year from baseline decreasing further to 11% energy difference at 9 years. Results The participants’ mean age was 62.3 years, 3.4% reported instances of CVD. In comparison to the participants in the control group those in the intervention group reported significant changes in dietary components paving way for 8.2% lower mean total fat intake and 2.9% lower saturated fat intake which includes decreased intake of trans, mono- and polyunsaturated fat and cholesterol intake with increased consumption of fruits, vegetables, fibre, whole grains and soy. At the end of trial, 2404 women (4.9%) died, 1553 (3.2%) stopped follow-up and 527 (1.1%) were lost to follow-up. 5% in the intervention group and 4% in the control group withdrew, were lost to follow-up or stopped providing answers for more than 18 months during the study period. At 3 years of follow-up, women in the intervention group showed significant decrease in body weight, waist circumference diastolic blood pressure and LDL-C level but showed no effect on triglycerides and HDL-C levels, ratio of total cholesterol to HDL-C, levels of non-HDL-C, lipoprotein, glucose or insulin or insulin resistance as reported by homeostasis. Carotenoid levels that denotes increased vegetable consumption was significantly higher. After 8.1 years of follow-up, major CHD incidence levels were 30% lower in the intervention group compared to the control group. Dietary intervention did not bring in significant changes in major CHD or composite CHD rates. Neither total, fatal or nonfatal stroke were influenced by dietary intervention nor were composite measure of CVD. There seemed to be no influence on stroke levels even after 9 years of follow-up and only a nonsignificant trend towards decreased CHD rates in the intervention group in the later years. The WHI trial reduced fat intake by 8.2% at the end of 6 years while increasing vegetable and fruits servings by 1.1 and whole grain servings by 0.5. The trial decreased fat intake and increased produce intake modestly only and did not show any reduction in risk of CHD or stroke. Diabetes & Heart Disease Risk in Postmenopausal Women 83% participants in the WHI trial agreed for non-intervention follow-up and 86% of participants consented to an open-end follow-up. Analyses over the intervention and cumulative follow-up period identified significant intervention benefits related to breast cancer, CHD and diabetes. Cancer outcomes were coded the US National Cancer Institute’s SEER system throughout the intervention and postintervention phases. CHD was defined as nonfatal myocardial infarction plus CHD death. Total stroke was defined as ischemic plus haemorrhagic stroke. Total CVD was defined as CHD plus coronary artery bypass graft or percutaneous coronary intervention plus total stroke. Results showed that fat intake was lower by 11% in the intervention group, carbs intake higher by 10% and protein intake by almost 1%. Vegetable and fruits intake were higher by 1.2 servings to 5.1/d and grains was higher by ∼0.7 servings to 5.4/d in the intervention group. There was a significant reduction in breast cancer risk by 30% followed by death due to any cause. There was also a significant reduction in estrogen receptor positive, progesterone receptor negative and breast cancer incidence over the long-term follow-up. There were 13,498 deaths that happened during this period. A significant reduction in CHD rates happened among baseline normotensive participants while there was no effect seen on hypertensive participants. Total fat reduction in the follow-up of postmenopausal women showed that reduction in total fat was accompanied by increased vegetables, fruits and grains with increases in fiber and total carotenoid intakes. There were small but significant changes observed in blood pressure, LDL cholesterol, insulin, glucose, HOMA-IR and metabolic syndrome score that could help with CHD and diabetes risk. Replacing fats with carbs in a well-nourished population of postmenopausal women showed ∼24% of energy from fats compared with ∼35% in the comparison group, ∼58% of energy from carbohydrates compared with ∼48% in the comparison group and ∼18% compared with 17% of energy from proteins. While consumption of saturated and unsaturated fats decreased among participants the intervention group started eating more of fruits, vegetables, whole grains, micronutrients and fiber along with increase in sugars. Such dietary modifications proved beneficial for participants at a risk for CHD, diabetes and stroke. Hence, dietary changes decreased breast cancer risk by ∼35% during intervention and 15% over cumulative follow-up; reducing in CHD incidence by ∼30% during intervention and 15% over the cumulative follow-up among normotensive women and reduction in insulin-requiring diabetes by ∼25% during the intervention and 13% over cumulative follow-up. References Low-fat Dietary Pattern & Risk of Cardiovascular Disease: https://jamanetwork.com/journals/jama/fullarticle/202339 Low-fat Dietary Pattern Among Postmenopausal Women Influences Long-term Cancer, Cardiovascular Disease and Diabetes Outcomes: https://academic.oup.com/jn/article/149/9/1565/5512736  Eating Rainbow-colored Produce Adds Goodness to Health Eating Rainbow-colored Produce Adds Goodness to Health The early man survived basically on hand-picked fruits, vegetables and nuts (besides hunting down animals) before the discovery of fire. Our ancestors were one of the strongest beings who existed on Earth as they relied mostly on natural produce, pulses and grains to satisfy hunger cues. This is more than enough to reinstate the fact that eating aplenty fruits and vegetables forms the basis for a good healthy life. Even today, doctors advise patients to eat a well-balanced diet where one-half of the plate is filled with veggies and fruits only. But not one single fruit can accomplish all nutrient requirements and we need to eat a variety of colourful fruits and veggies to acquire all the goodness and nutrition of the different foods. A diet rich in fruits and veggies has the potential to lower blood pressure, reduce the risk of heart disease and stroke, prevent some types of cancer, lower risk of eye and digestive problems and also benefit blood sugar levels that in turn can keep one’s appetite in check. The choice of the fruit can also have a great impact on the benefit that you reap. For instance, non-starchy fruits such as apples, pears and green leafy vegetables might promote weight loss as these fruits have low glycemic loads that prevent blood sugar spikes (this can increase hunger levels amounting to weight gain). There are at least nine different families of fruits and vegetables each of which have hundreds of different plant compounds that are beneficial to health. What we choose and how we eat are key players in adding benefits to our body. Fruits, according to the Dietary Guidelines for America (DGA) is a nutrient-dense food that’s to be included as part of a healthy eating pattern and consuming them helps individuals balance nutrient needs with energy needs. Quantity recommendations depend on age, gender and physical activity levels: for kids it ranges from 1 cup for 2-3 years of age going up to 2 cups for males 14-18 years of age. While its suggested fresh, frozen, canned or dried fruit can be consumed to meet recommended quantities and so can 100% fruit juice my personal suggestion would always be fresh whole fruits as they are enriched in fibre content and provide maximized benefits. Almost 30-50% total fruit intake by kids aged between 9 and 18 years comes from 100% fruit juice and this has also increased their whole fruit consumption and improved overall diet quality. Despite various benefits and different forms available for consumption 75% kids aged between 9 and 13 years don’t meet recommended levels. Individuals these days lack in a number of nutrients such as fibre, potassium and vitamins, and fruits are indeed rich in all of them apart from being a rich source of phytochemicals making these foods indispensable for a healthy body. An Apple a Day Keeps Nutrition at Bay Apple is one of the commonest fruits consumed by almost everyone and it is available throughout the year irrespective of the season. One medium raw apple with skin contains 95 kcals, 19g of total sugar, 4g dietary fibre and 195 mg of potassium with almost close to zero total fat, saturated fatty acids, sodium and cholesterol. Processed apple products don’t have the same nutrient content as its raw form. For instance, apple sauce may or may not have added sugars and ½ cup has only 1.3 g of dietary fibre while 100% fruit juice contains even less-0.2 g of dietary fibre. Still, every apple product contributes towards total fruit intake through the day. Despite apples also being rich sources of phenolics, especially hydroxycinnamic acid derivatives and flavonoids not many kids love to eat this fruit regularly! Apple Peel Might Diminish Obesity Rates Most fruits are edible with their peel and we have often heard our parents insist that we eat the fruit with the peel to experience 100% nutrient value. A study by researchers at the University of Iowa shows that a natural substance found in apple peel can partially protect the mice from obesity and some of its harmful effects. According to the researchers, the study identified that a substance known as ursolic acid reduced obesity and other health problems by increasing muscle and brown fat, two tissues that are well-known for their calorie-burning properties. The study tested ursolic acid on mice on a high-fat diet and found that it increased skeletal muscle while reducing obesity, pre-diabetes and fatty liver disease. Half of the mice received ursolic acid in their high-fat food and these mice actually ate more food than mice not getting any supplements and there was no difference in activity found between the two groups. Still, the mice that received ursolic acid supplement gained less weight and blood sugar levels also remained near normal besides the fact that these mice also did not develop obesity-related fatty liver disease, a condition that affects almost 1 in 5 Americans. We know that muscle is an excellent source for burning calories and the research proves beyond that increased muscle in ursolic-acid treated mice helped in lowering obesity. Ursolic acid also increases brown fat, another excellent source to burn calories and prevent obesity. While it was believed until now that only infants had brown fat studies show that even adults have very small quantities in the neck and between shoulder blades. The current research also showed that ursolic acid consumption improved skeletal muscle (increasing endurance and strength) and quantity of brown fat. Hence, the presence of ursolic acid improves calorie burning and in turn prevents obesity, pre-diabetes and fatty liver disease, and apple peel contains this nutrient. Apple Consumption Satisfies Various Nutrient Requirements in Kids There have been no studies until now that examined the association between apple consumption and diet quality in kids and the study below examines the association between them using the National Health and Nutrition Examination Survey (NHANES). The NHANES provides information about kids in the form of interviews, dietary intake and physical examinations. The study consisted of 13,339 kids aged between 2 and 18 years who participated in the survey from 2003-2010. The participants’ consumption of apple/apple products was determined from a 24-h dietary recall that included whole apples, apple sauce (includes cooked apples), 100% apple juice and total apples (all foods from all these three apple groups). The Healthy Eating Index (HEI-2010) was used to determine diet quality score where 9 of 12 components that included fruits, vegetables, greens, beans, whole grains, dairy, total protein foods, seafood and plant proteins and fatty acids measure adequacy with higher scores while three other components including refined grains, sodium and empty calories must have higher scores as in this case, a higher score indicates lower consumption. Each of the participant’s height, weight, BMI and waist circumference was measured and kids were categorized according to results: those with a BMI value ≥85th and <95th percentile were considered overweight and kids ≥95th percentile were considered obese. The study showed that almost 26% of population consumed one or the other form of apple product, 14% consumed whole apples, 5% consumed apple sauce and almost 12% consumed 100% apple juice. Most of the children who consumed apple products were younger and less likely to be current smokers. Results showed that:
References Apple Peel Compound Boosts Brown Fat, Reduces Obesity in Mice: https://www.sciencedaily.com/releases/2012/06/120620212855.htm Consumption of Apples is Associated with Better Diet Quality & Reduced Risk of Obesity in Children: https://nutritionj.biomedcentral.com/articles/10.1186/s12937-015-0040-1 Vegetables and Fruits: https://www.hsph.harvard.edu/nutritionsource/what-should-you-eat/vegetables-and-fruits/ |
AVOID FRAUD. EAT SMART+91 7846 800 800
|
- Home
- Written Testimonials
- Consult
- Clinics
- Blogs
-
Diet & Nutrition
- Diabetes Reversal
- IVF IUI not needed for PCOS PCOD Infertility
-
Medical Nutrition
>
-
Disease & Conditions
>
- Infertility | PCOS
- Diabetes Mellitus
- Cholesterol
- Hypothyroid
- Kidney Problems
- Hypertension
- Cardiovascular Diseases
- Liver Diseases
- Gastro intestinal disorder
- Cancer
- Metabolic Disorders
- Orthopedic Disorders
- Eating Disorders
- Dietary Recall
- Weight Record Filled By Clients
- Online Payment Transaction Details
- Online Clients Weight Check Form
- Our Program Package Service Charges
- Weight Record 2017 Clients
- Measurements sent by Clients
- Terms & Conditions Of Payment
- Thanks. Your Form is Submitted
- Video Testimonials
- Lifestyle & Wellness
- Lifestyle & Wellness Blog
- Allergy & Intolerance
- Weight Loss / Gain
- Weight Loss / Slimming Blog
-
Disease & Conditions
>
- Life Cycle Nutrition >
- Sports Nutrition >
- Integrity in Nutrition
- Knowledge Centre
© COPYRIGHT 2022. ALL RIGHTS RESERVED. FRST HEALTHCARE PVT LTD.
Dr. Nafeesa Imteyaz of First Eat Right clinic, is the Best Dietitian Nutritionist in Bangalore. Best Dietitian Nutritionist in Pune. Best Dietitian Nutritionist in Hyderabad. Best Dietitian Nutritionist in Chennai. Best Dietitian Nutritionist in Mumbai. Best Dietitian Nutritionist in Delhi. Best Dietitian Nutritionist in Kolkata.